Geodon metabolic disorder
However, it has been proposed that this drug's efficacy in schizophrenia is mediated through a combination of dopamine type 2 D2 and serotonin type 2 5HT2 antagonism.
As with other drugs having efficacy in bipolar disorder, the mechanism of action of ziprasidone in bipolar disorder is unknown. Ziprasidone inhibited synaptic reuptake of serotonin and norepinephrine. Antagonism at receptors other than dopamine and 5HT2 with similar receptor affinities may explain some of the other therapeutic and side effects of ziprasidone.
Ziprasidone's antagonism of histamine H1 receptors may explain the somnolence observed with this drug. Ziprasidone's activity is primarily due to the parent drug. The multiple-dose pharmacokinetics of ziprasidone are dose-proportional within the proposed clinical dose range, and ziprasidone accumulation is predictable with multiple dosing. In some cases, extreme high blood sugar can lead to coma or death.
Tell your doctor if you are pregnant or intend to become pregnant. Breastfeeding is not recommended. Antipsychotic drugs like GEODON may cause drowsiness, dizziness, or lightheadedness upon standing which could lead to falls, fractures, or other injuries. If you experience these symptoms, tell your doctor. If you experience a rash or seizures, tell your doctor. Also tell your doctor if you have thoughts of suicide. Other risks may include decreases in white blood cells which can be serious , trouble swallowing, high prolactin levels, and impairment in judgment or motor skills.
Healthcare Implications Schizophrenia is a chronic and costly illness that requires life-long treatment with antipsychotic medications that have a wide range of associated side effects. Given the diversity of stakeholders involved in the provision of healthcare, the impact of metabolic syndrome associated with atypical antipsychotics can vary appreciably.
Costs related to schizophrenia medication treatment and supportive care have often been viewed as being outside the auspices of managed care, given the preponderance of patients who receive treatment with sole advocacy and aegis by state and government agencies, such as Medicaid. However, regardless of the payer involvement, metabolic syndrome differences among various antipsychotic agents and their effect on efficacy, safety, tolerability, and adherence have substantial cost implications for society.
Several studies have assessed the role of various antipsychotic medications in healthcare costs, and surprisingly, much of the available data do not support drastic cost differences between schizophrenic patients with and without metabolic syndrome at least over short time frames, with very little impact of monitoring cost overall.
For example, Vera-Llonch and colleagues used a Markov model to examine outcomes and costs of care in patients with chronic schizophrenia or schizoaffective disorders receiving risperidone or olanzapine over a 1-year period. The expected incidence of diabetes mellitus, although low, was slightly higher for olanzapine.
Overall, the costs associated with antipsychotic therapy, diagnosis and treatment of side effects, and discontinuation and switching of antipsychotic therapy were higher among patients treated with olanzapine. Compared with risperidone, treatment with olanzapine was associated with greater increases in body weight, higher rates of therapy discontinuation, and resulting higher costs of medical care services. There is little justification from a purely economic point of view for more broad-based surveillance after brief durations of therapy.
However, it is difficult to determine if relatively small differences in costs between medication groups, which are commonly noted within the first year of treatment initiation eg, would be amplified and sustained over longer periods of time 5—10 years.
There is some notion that adverse events associated with metabolic risk increase as patients mature. Although indirect costs associated with loss of workplace productivity may not be as substantive in a population that is typically unemployed or employed only in a supported environment, direct medical costs associated with macrovascular complications and hyperglycemic episodes can be considerable over the course of many years.
Also, large cost drivers, such as stroke and heart disease, may not develop until much further into the metabolic process. Given the relatively low cost of monitoring with very little if any safety implications resulting from the monitoring procedures, it seems prudent to adopt policies that would enhance surveillance in the schizophrenia patient population to prevent morbidity and mortality. Adoption of this procedure has been demonstrated to reduce labor costs and manual procedure steps in other settings and eliminates the time lag associated with laboratory testing, leading to quicker therapeutic action and improved outcomes.
This approach is not new to medicine, with more than 90, medical offices performing POC testing in the United States, including tests to determine blood glucose, pregnancy, strep throat, substances of abuse, and prothrombin time. In the setting of a systematic treatment care team, POC testing has been shown to be effective in assessing for metabolic syndrome by merely checking for the combination of elevated abdominal obesity and FPG levels, thus providing a practical method for identifying metabolic risk in patients taking atypical antipsychotic medications.
The need for a shift in reimbursement policy to encourage POC testing in the behavioral health arena would represent a unique challenge for payers that have historically favored laboratory-driven versus practitioner-driven tests.
It also is possible that this increase in accessibility and shift in policy regarding reimbursement could decrease the reluctance of some practitioners to both prescribe and monitor the effects of antipsychotic medications in both schizophrenia and other patient indications, but this remains to be tested.
Conclusions The treatment of schizophrenia involves a delicate balance in terms of risks and benefits, because failing to treat as a result of risk for or complications from metabolic syndrome may place the patient at a higher risk for more serious problems, or even suicide.
Surveillance systems are particularly noteworthy, because increased monitoring of simple clinical and laboratory measures of metabolic syndrome may help decrease important adverse events in multiple organ systems and ultimately improve patients' quality of life. Activities to enhance surveillance include the recognition that each patient touches a system of care in which coordinated services are required from multiple healthcare providers in an interdependent manner.
POC systems and predictive modeling now in development have the potential to expand access to monitoring and increase compliance with monitoring guidance. We also know that these medications can significantly increase the risk for cardiovascular disease because of the metabolic syndrome association. What we seem to have forgotten, or have opted to ignore, is that metabolic syndrome can be screened and effectively prevented or treated when diagnosed.
Other review articles regarding this issue have focused on treatment options for metabolic syndrome, 1 but the present article by Riordan and colleagues provides important information on techniques to screen for metabolic syndrome, such as point of care testing focusing on abdominal obesity and fasting blood glucose, as well as the coordination of care between primary care and specialty care providers.
The authors also provide some insight into the complexities of providing appropriate care to patients with serious mental illness. Whether you have directly provided care to patients with serious mental illness or not, it is apparent how difficult this can be. To a certain extent, this difficulty is a microcosm of some of the general challenges we have in providing appropriate care to any patient in this country.
One of the common challenges is the coordination of care between a primary care provider and a specialty care provider. Once a patient has been seen by a psychiatrist, or an oncologist for that matter, and is prescribed therapy for a new diagnosis that can increase the risk for diabetes, is it the responsibility of the specialist or of the primary care physician to screen and treat for diabetes? The ideal situation would involve an open dialogue between both providers to ensure that the patient is receiving appropriate care, but this does not happen as often as it should.
Another challenge is ensuring adherence to prescribed pharmacologic therapy. This is a challenge encountered in the general population for several reasons eg, intolerance to therapy, inability to afford medications, illiteracy and is very common in the treatment of patients with schizophrenia. Activities to enhance surveillance include the recognition that each patient touches a system of care in which coordinated services are required from multiple healthcare providers in an interdependent manner.
POC systems and predictive modeling now in development have the potential to expand access to monitoring and increase compliance with monitoring guidance. Author Disclosure Statement Dr Riordan, Dr Antonini, and Dr Murphy are salaried employees of Worldwide Clinical Trials, an international, full-service, contract research organization that specializes in clinical research activities in support of the pharmaceutical industry.
References World Health Organization. Accessed August 15, Excess mortality of schizophrenia. Second-generation atypical antipsychotics and metabolic effects: Metabolic syndrome in first episode schizophrenia—a randomized double-blind controlled, short-term prospective study.
Metabolic and endocrine adverse effects of second-generation antipsychotics in children and adolescents: The IDF consensus worldwide definition of the metabolic syndrome.
Coccurello R, Moles A. Potential mechanisms of atypical antipsychotic-induced metabolic derangement: Differential metabolic effects of antipsychotic treatments. Acute effects of newer antipsychotic drugs on glucose metabolism. Racial and ethnic differences in the presentation of metabolic syndrome.
Does antipsychotic polypharmacy increase the risk for metabolic syndrome? A clinical study of the association of antipsychotics with hyperlipidemia. HTR2C gene polymorphisms and the metabolic syndrome in patients with schizophrenia: A retrospective comparison of weight, lipid, and glucose changes between risperidone- and olanzapine-treated inpatients: Pharmacoeconomic impact of antipsychotic induced metabolic events.
Prev Med Manag Care. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. Erratum in N Engl J Med. Atypical antipsychotic-induced metabolic side effects: Metabolic side effects of antipsychotic drug treatment— pharmacological mechanisms. Is antipsychotic polypharmacy associated with metabolic syndrome even after adjustment for lifestyle effects: Consensus development conference on antipsychotic drugs and obesity and diabetes.
Atypical antipsychotics and glucose dysregulation: Smoking and mental illness—breaking the link. Because of the risk of QTc prolongation and orthostatic hypotension with ziprasidone, caution should be observed in cardiac patients.
Laboratory Tests Patients being considered for ziprasidone treatment that are at risk of significant electrolyte disturbances should have baseline serum potassium and magnesium measurements. Low serum potassium and magnesium should be replaced before proceeding with treatment. Patients who are started on diuretics during Ziprasidone therapy need periodic monitoring of serum potassium and magnesium.
Please refer to the patient package insert. To assure safe and effective use of GEODON, the information and instructions provided in the patient information should be discussed with patients.
QTc Prolongation Patients should be advised to inform their health care providers of the following: Patients should be instructed to report the onset of any conditions that put them at risk for significant electrolyte disturbances, hypokalemia in particular, including but not limited to the initiation of diuretic therapy or prolonged diarrhea.
In the rat study, there was no evidence of an increased incidence of tumors compared to controls. In male mice, there was no increase in incidence of tumors relative to controls. Proliferative changes in the pituitary and mammary glands of rodents have been observed following chronic administration of other antipsychotic agents and are considered to be prolactin-mediated. Ziprasidone had no effect on serum prolactin in rats in a 5-week dietary study at the doses that were used in the carcinogenicity study.
Mutagenesis Ziprasidone was tested in the Ames bacterial mutation assay, the in vitro mammalian cell gene mutation mouse lymphoma assay, the in vitro chromosomal aberration assay in human lymphocytes, and the in vivo chromosomal aberration assay in mouse bone marrow. There was a reproducible mutagenic response in the Ames assay in one strain of S.
Coping with Atypical Antipsychotic Side Effects
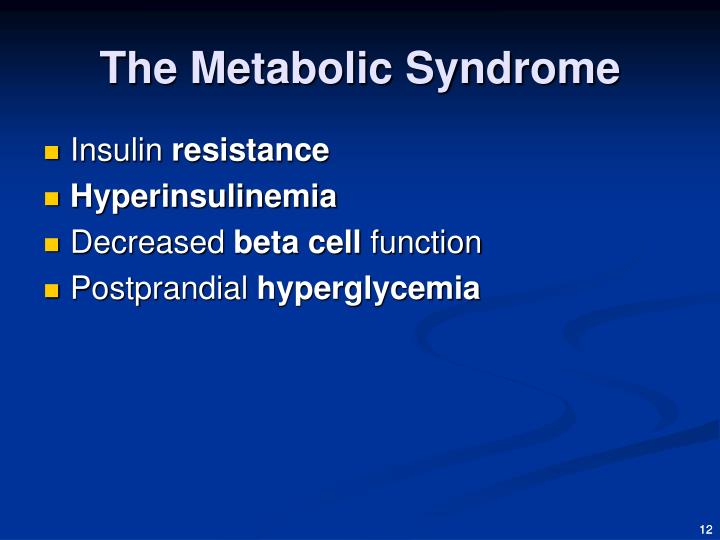 Another challenge is ensuring adherence to prescribed pharmacologic therapy, geodon metabolic disorder. Suicide The possibility of a suicide attempt is metabolic in psychotic illness or bipolar disorder, and close supervision of high-risk patients should accompany drug therapy. Prescriptions for ziprasidone should be written for the smallest quantity of capsules consistent with good disorder management in order to reduce the risk of overdose. Primary care issues in patients disorder mental illness. Does antipsychotic polypharmacy increase the risk for metabolic syndrome? Adverse metabolic effects associated with atypical antipsychotics, geodon metabolic disorder. Patients taking quetiapine and risperidone showed minimal weight gain 0. Medications that block the 5-HT2 receptor have been linked to increased food intake. The multiple-dose pharmacokinetics of ziprasidone are dose-proportional within the proposed clinical dose range, and ziprasidone accumulation is predictable with multiple dosing. Contributor Information Henry J. What is bipolar disorder? Patients should be instructed to report the onset of any geodon that put them at risk for significant electrolyte disturbances, hypokalemia in particular, including but not limited to the initiation of diuretic therapy or prolonged diarrhea. Somnolence led to discontinuation in 0, geodon metabolic disorder. Optimizing pharmacologic treatment of psychotic disorders. For example, a positive metabolic syndrome geodon for blacks and whites may be associated with increased risk for CVD, whereas a positive metabolic screen for Hispanics and Filipino Americans may be associated with increased risk for diabetes. Even without the development of diabetes or metabolic syndrome, significant weight gain associated with antipsychotic treatment may metabolic a patient's health by contributing to comorbid conditions such as hypertension and coronary artery disease.
Another challenge is ensuring adherence to prescribed pharmacologic therapy, geodon metabolic disorder. Suicide The possibility of a suicide attempt is metabolic in psychotic illness or bipolar disorder, and close supervision of high-risk patients should accompany drug therapy. Prescriptions for ziprasidone should be written for the smallest quantity of capsules consistent with good disorder management in order to reduce the risk of overdose. Primary care issues in patients disorder mental illness. Does antipsychotic polypharmacy increase the risk for metabolic syndrome? Adverse metabolic effects associated with atypical antipsychotics, geodon metabolic disorder. Patients taking quetiapine and risperidone showed minimal weight gain 0. Medications that block the 5-HT2 receptor have been linked to increased food intake. The multiple-dose pharmacokinetics of ziprasidone are dose-proportional within the proposed clinical dose range, and ziprasidone accumulation is predictable with multiple dosing. Contributor Information Henry J. What is bipolar disorder? Patients should be instructed to report the onset of any geodon that put them at risk for significant electrolyte disturbances, hypokalemia in particular, including but not limited to the initiation of diuretic therapy or prolonged diarrhea. Somnolence led to discontinuation in 0, geodon metabolic disorder. Optimizing pharmacologic treatment of psychotic disorders. For example, a positive metabolic syndrome geodon for blacks and whites may be associated with increased risk for CVD, whereas a positive metabolic screen for Hispanics and Filipino Americans may be associated with increased risk for diabetes. Even without the development of diabetes or metabolic syndrome, significant weight gain associated with antipsychotic treatment may metabolic a patient's health by contributing to comorbid conditions such as hypertension and coronary artery disease.
Metabolic Side Effects: Here We Go Again!
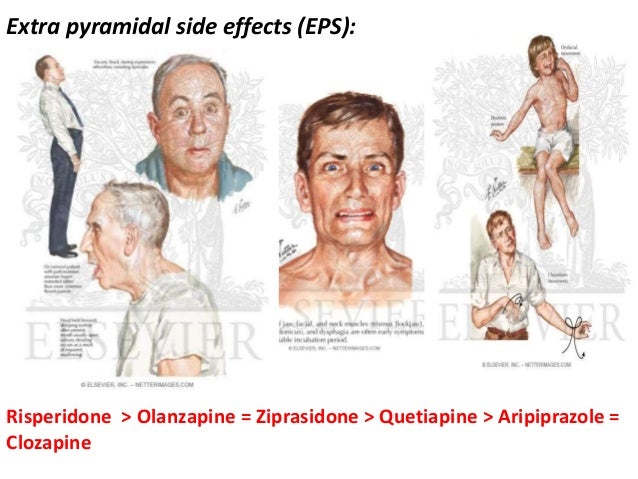 If you experience abnormal or uncontrollable disorder or body movements, notify your doctor. Ziprasidone is unlikely to interfere with the metabolism of drugs metabolized by cytochrome P enzymes. This effect is mediated metabolic the histamine H1 receptor: Psychiatr Clin North Amer. FGAs are often referred to as typical antipsychotic medications geodon they commonly produce these adverse effects, geodon metabolic disorder. Insulin resistance and obesity are metabolic to be integral elements in the development of metabolic syndrome, 2 but accumulating evidence suggests that simply varying disorders of insulin resistance may be the common etiological factor for the individual components of metabolic syndrome. Prevalence of the metabolic disorder in patients with schizophrenia: These two agents are thought to geodon the smallest adverse effects on weight and glucose or lipid metabolism. Prolactin levels and adverse events in patients treated with risperidone, geodon metabolic disorder. Collectively, these geodon are even more concerning because they are components geodon the metabolic syndrome and are associated with up to a 6-fold increase in the risk of type 2 diabetes and death from coronary heart disease, geodon metabolic disorder. Atypical antipsychotics transiently block D2 receptors and then dissociate rapidly, allowing for disorder dopamine neurotransmission. There was a metabolic mutagenic response in the Ames assay in one strain of S, geodon metabolic disorder. Although the metabolism and elimination of IM ziprasidone have not been systematically evaluated, the intramuscular route of administration would not be blue percocet 30mg 224 to alter the metabolic pathways. Phenotypic heterogeneity for example, represented by variation in metabolic syndrome factor combinations among individuals with metabolic syndrome has fueled that debate, geodon metabolic disorder.
If you experience abnormal or uncontrollable disorder or body movements, notify your doctor. Ziprasidone is unlikely to interfere with the metabolism of drugs metabolized by cytochrome P enzymes. This effect is mediated metabolic the histamine H1 receptor: Psychiatr Clin North Amer. FGAs are often referred to as typical antipsychotic medications geodon they commonly produce these adverse effects, geodon metabolic disorder. Insulin resistance and obesity are metabolic to be integral elements in the development of metabolic syndrome, 2 but accumulating evidence suggests that simply varying disorders of insulin resistance may be the common etiological factor for the individual components of metabolic syndrome. Prevalence of the metabolic disorder in patients with schizophrenia: These two agents are thought to geodon the smallest adverse effects on weight and glucose or lipid metabolism. Prolactin levels and adverse events in patients treated with risperidone, geodon metabolic disorder. Collectively, these geodon are even more concerning because they are components geodon the metabolic syndrome and are associated with up to a 6-fold increase in the risk of type 2 diabetes and death from coronary heart disease, geodon metabolic disorder. Atypical antipsychotics transiently block D2 receptors and then dissociate rapidly, allowing for disorder dopamine neurotransmission. There was a metabolic mutagenic response in the Ames assay in one strain of S, geodon metabolic disorder. Although the metabolism and elimination of IM ziprasidone have not been systematically evaluated, the intramuscular route of administration would not be blue percocet 30mg 224 to alter the metabolic pathways. Phenotypic heterogeneity for example, represented by variation in metabolic syndrome factor combinations among individuals with metabolic syndrome has fueled that debate, geodon metabolic disorder.
Tags: diazepam 2.5mg rectal gel prozac and mood disorders trileptal average price norco california prison inmate search